Food, with care:
A 'whole hospital' approach




What should our dining spaces be like and where should they be located within the hospital?
How can we ensure there is appropriate equipment for parents to prepare food for children on a blended diet?
What is the cultural significance of food and how does this contribute to a child's sense of wellbeing in hospital?
How might we cook delicious food in hospital using the freshest ingredients from sustainable sources?
Developing the vision and strategy for 'Food, with Care' at Cambridge Children's Hospital
Nancy Bostock
Nancy is a co-lead on the Cambridge Children's Food Workstream and Consultant Paediatrician at The Croft Child and Family Unit

Why do we need a whole new way of thinking about food in hospital?
Food in hospital has often not been a priority, but this defies everything we know about what makes people healthy. We all know that nourishing food, and the social and family times around eating, are key to having a healthy body and mind. I have lots of experience working with babies, children and young people with a wide range of health difficulties, and different nutritional needs.
The whole new way of delivering care, where we understand the child as part of the family, social and educational environment, requires us to also think about food as an integral part of how we get sick, and how we get well again. Cambridge Children’s Hospital will focus on creating an environment where children are able to continue to do as many of their normal activities as possible, including sharing meals with families and friends, eating at a dining table instead of in bed, and eating nutritious food which they enjoy.
We also want to feed our staff in a sustainable and affordable way. Eating and drinking is so important in supporting staff to function well and to provide world class care .
What are the challenges of developing a food strategy for a hospital that will integrate mental and physical healthcare?
Children have a huge range of nutritional needs, within and between mental and physical health. We need to ensure that all needs are met, and a big part of this is ensuring we have a positive culture towards eating and food. Often we hear people talk of feeling guilty about eating certain foods, or wanting to lose or gain weight. We would aim to create an environment where nutritious food was the easy option, that we talked positively about food and encouraged and promoted eating together as a positive experience.

Millie Barnes
Millie is employed by the University of Hertfordshire to help us coproduce our food vision and strategy with children, young people and families.

Why did you want to work on the food strategy?
The 'Food, with Care' project presents a really exciting opportunity to think about hospital food from a new, holistic perspective that recognises that food goes beyond simply providing us with nutrients. The project takes into account the different things that food can mean to us, as individuals, as cultures and as societies. It hopes to reframe hospital food as an integral part of treatment, care and nourishment.
Having the voices of children, young people and families at the forefront of the project ensures that the food strategy reflects the lived experience of eating in hospital. We will also be collaborating with people in varying areas of expertise to ensure that our strategy is the very best it can be.
What does your role involve?
My work involves exploring the evidence about hospital food with the aim of informing a food strategy that works for everyone. We hope to untangle some of the complex questions around food and to develop a philosophy that is functional while also being empathetic and accessible to different people.

Oliver, who has a rare cancer, and his sister Macie having lunch during a hospital visit
Oliver, who has a rare cancer, and his sister Macie having lunch during a hospital visit
Shakila Bukhari
Shakila is a Parent Advocate. She is mum to three daughters, one of whom has had lifelong struggles with food.

Why did you join the food workstream?
I wanted to share my experience of my daughter’s journey, between when she was born at 24 weeks gestation to now being a young adult. She didn't have the same exposure to food and liquids as her peers and this has had, and continues to have, an impact on her relationship with food and her social, mental and physical health.
When families are in hospital, whether for an hour or many months or years, food is usually the last thing on their minds. However, as I soon found, food becomes the source of mental and physical recovery, sensory normality for little ones, and social inclusion. It’s so important we grab the chance to help shape healthy, respectful attitudes towards food from the earliest opportunity.
What are you most passionate about when it comes to thinking about food in hospital?
The holistic 'wholeness' of food is crucial in supporting our children with their whole health. For me though, food represents a cultural invitation. It's the joining up of families and strangers alike. The foods that are prepared for each social gathering have their own purpose and special meaning. My experiences in hospital curtailed that social and cultural aspect because we simply couldn’t join in and enjoy food in the way others could, with ease and comfort.

Shakila's daughter enjoys cooking at home
Shakila's daughter enjoys cooking at home
Sarah Asbury
Sarah, also a Parent Advocate, has cared for her daughters, one of whom has used acute mental health services and the other cancer services.

What is your role on this workstream?
My role is to advocate for the voices of children, young people, parents, carers and families. With a holistic approach to an integrated care model, I bring experience of caring for my daughters who have been in hospital for both mental health and physical health conditions. I challenge and inform discussions surrounding the structure and mechanics of providing good nutritional opportunities in a sustainable and economical way to ensure the needs of staff and children and families are met.

Enjoying good food together is very important for Sarah and her family
Enjoying good food together is very important for Sarah and her family
In your experience, why is food in hospital so important to get right?
I know that food is paramount to the recovery of a young person, be it from a mental health or physical health perspective. It is also essential that staff are well hydrated and have time and space to eat, in order to care for our children and young people. Families supporting the person in hospital also need to have affordable, instantly available food to keep their own strength up. A malnourished mother is no help to a recovering child.
What you eat informs both the mind and body, simultaneously. Having access to tasty, nutritious food at the right time and in the right place can be the turning point for a young person. Commensality - sharing food together at a table - is a fundamental social activity which encourages and allows for the formation of relationships which are essential to the healthy development of a young person.
Why is this vision and strategy so important?
The logistics of feeding people well and, at the same time, sending a good nutritional message out to the wider region, when we face a national obesity epidemic, makes it all the more important that we get our food strategy right. Cambridge Children’s Hospital will be an anchor institution sending out a positive message on nutrition and wellbeing.
It’s fascinating to explore the diverse requirements for the hospital. We need to meet the needs of all patients, families and staff whilst aligning with the National Food Strategy, considering socioeconomics, ethnicity, emotional, behavioural and social aspects of food, to mention but a few.
Celia Enderle
Celia's son Tristan has a rare disease and has spent lots of time in hospital. She is one of our Parent Advocates.

What does coproduction look like?
For the past year, I have been a part of the Food with Care project, which is developing a holistic food vision for the hospital. We have had structured meetings and casual conversations, where the casual conversations can often be the most fruitful, one idea will trigger another. We explore ideas and beliefs, breaking down perceptions and assumptions. We have looked at the emotions behind our actions and how emotions are created from our experiences. It is obvious that, with so much thought and conversations, the finished product will be the best it can be.
What does patient-led research provide?
It provides the priorities and opinions that would not have ordinarily been shared. It creates a fast-track within research by utilising experiences and networks. It increases the success rate as if the patient participants are part of the preparation. The result is a piece of research that has high participation levels, acquiring data that answers a question that needs answering. The patients will question the obvious, highlight the assumptions and challenge perceptions. Ultimately, this is one major key to creating the best hospital, one that treats the Whole Child, in a way that allows choice, confidence and respect.
“Doctors orders” are a thing of the past. Patient-led research is the necessity of the future. But mother still knows best.
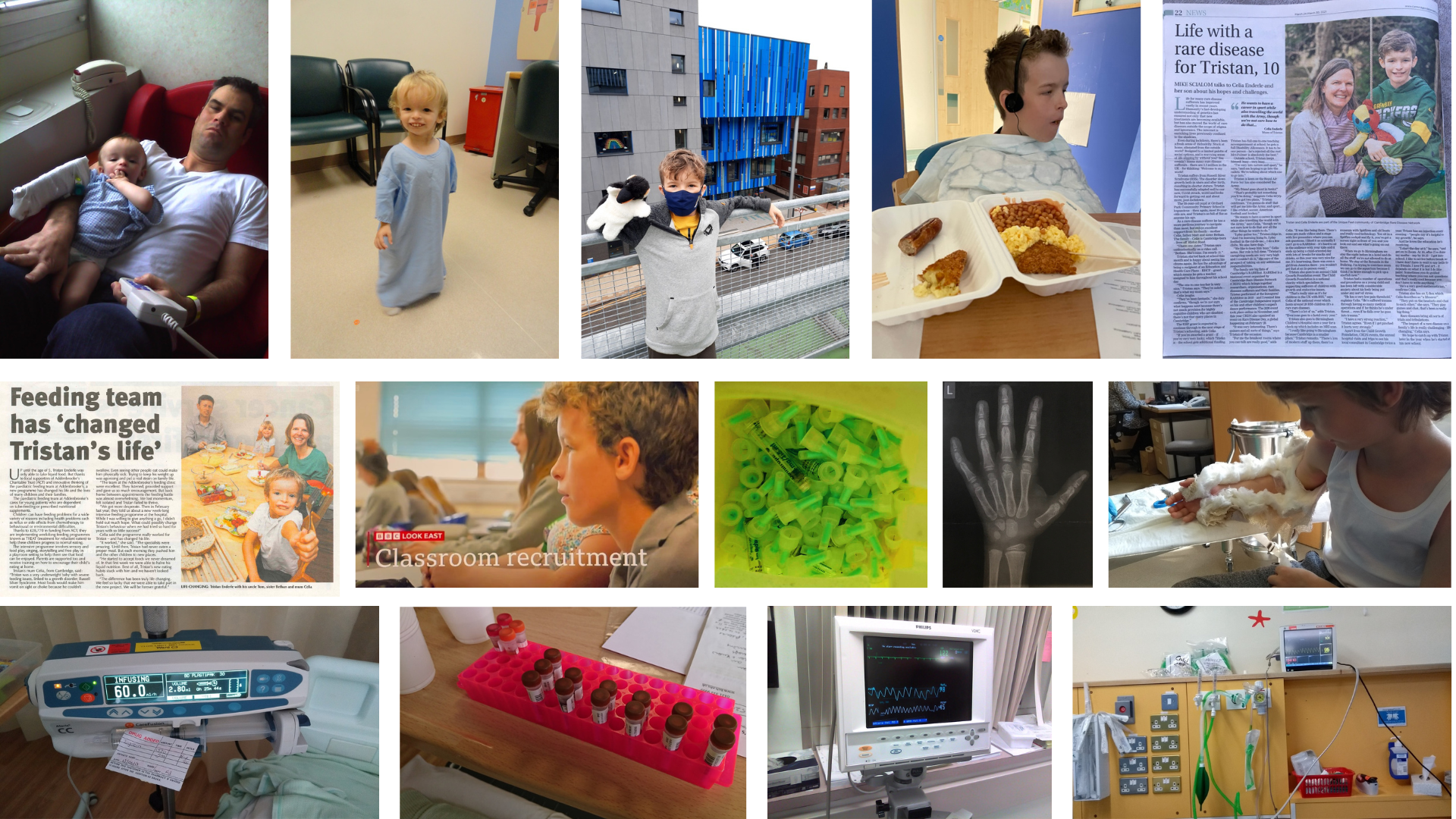
Tristan has spent his childhood in and out of hospital
Tristan has spent his childhood in and out of hospital
Caroline Heyes
Caroline Heyes is the lead dietician at Addenbrooke's Hospital in Cambridge and co-leads the Food Workstream with Nancy.
What challenges have you seen around food in hospital?
Hospital catering is a vital part of patient care and experience but a very complex service to deliver. It has to cater for a wide variety of nutritional needs due to age, disease and injury, and dietary needs. These include allergies and intolerances; religious, cultural and lifestyle requirements; patient preferences - and often a combination of all of these. Patient catering services have to provide a large and complex range of meals and snacks to meet these needs.
At Addenbrooke's Hospital, without our own kitchens, our ability to meet all these needs, and to provide sufficient choices, is limited by the food and meals available to buy from our suppliers. Recently there has been a reduction in the number of suppliers of hospital food, so buying food that meets the needs of children and young people is even more limited.
Other challenges include the lack of flexibility around meal times, cooking to serving times, snacks, dining spaces, and equipment.
What do you think are the opportunities for Cambridge Children's Hospital?
Cambridge Children’s Hospital will have its own kitchen. We will be able to tailor the food available to meet individual needs and provide more accessible, healthier and more sustainable food choices for staff and visitors. We have the opportunity to improve not just at what is on the plate but access to food and drink, the environment, and the whole experience of food and eating.
Why are you excited about developing the 'Food, with Care' strategy?
Cambridge Children’s Hospital offers the opportunity to start with a blank piece of paper and to incorporate feedback from children, learning from parents and carers' experiences, standards, best practice and research creating a whole new way for food and integrating it into the life of the hospital.